Coming of Phage
Western medicine long ago abandoned phage therapy, but it could become a key player in the fight against antimicrobial resistance, explain Timothy Lu and Robert Citorik
The Biologist 63(3) p12-15
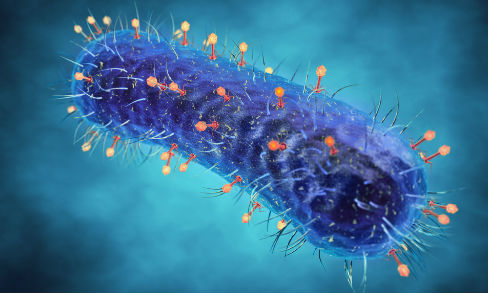
In an age when antibiotic-resistant bacterial infections are increasingly common and lead to more treatment failures, new solutions are sorely needed. One promising answer to these mounting concerns is a century-old solution forgotten by Western medicine that employs natural predators of bacteria: bacteriophages.
Like many antibiotics, bacteriophages (phages for short) are naturally occurring and have the capacity to kill bacteria. Unlike antibiotics, however, phages are viruses and so can replicate and amplify within their target bacteria. These 'bacteria eaters' are conceptually similar to human viruses, but can only infect bacterial cells. From a human perspective, phage therapy is a good example of the proverbial saying 'the enemy of my enemy is my friend'.
Phages reproduce by infecting bacteria and turning them into phage manufacturing plants, which can prove lethal to the bacterial cell. Once the progeny have been assembled, the phage initiates enzyme-mediated lysis, rupturing the host bacterium from the inside and releasing the next generation of infectious particles to repeat the cycle.
Phage therapy dates back to the early 20th century, shortly after the discovery of bacteriophages by English bacteriologist Frederick Twort (1915)[1] and French-Canadian Félix d'Hérelle (1917)[2] It was found that some natural element could yield zones of clearing on bacteria growing in Petri dishes or cause a healthy, cloudy culture of bacteria to suddenly lyse and become clear.
The lysed culture could be filtered and added to other cultures of the bacteria to cause a repeatable clearing effect. Phages able to lyse cultures of the intestinal pathogen Shigella were found alongside the bacteria in patients with dysentery, with an increase in phage concentration often corresponding to recovery, and so were thought to be part of the natural course of disease[3].
After some reported successes, research and commercial development of phage-based therapies expanded over the following decades, although there was still controversy surrounding the nature of the agent or agents causing the bactericidal effects. An early debate centred on whether phages were indeed of a viral nature or instead were autolytic enzymes produced by the bacteria themselves, and it was not until 1940 that electron micrographs were published visually depicting what was responsible.
In the beginning, scientists did not yet fully appreciate the diversity of phages and the specificity of each one to its target. Unlike broad-spectrum antibiotics, which kill bacteria fairly indiscriminately, phages are usually highly specific to a target bacterial species, and often limited to certain strains within a particular species.
Early experiments and trials were likely impacted by these and other gaps in knowledge, and choosing the wrong phages or using suboptimal phage preparations to treat a bacterial infection may have led to inconsistencies in treatment outcomes.
As a result, the initial excitement associated with phage therapy was short-lived. The appearance of antibiotics in the physician's toolbox around the mid-20th century coincided with a decline in phage therapy for various reasons, including the incredible efficacy of the new drugs, an insufficient understanding of phages and mixed reports of success, and even political motivations.
Despite the complicated history leading to phage therapy falling out of favour in the West[4], it has continued to some extent in other parts of the world, primarily in Russia and Eastern Europe. The George Eliava Institute of Bacteriophages, Microbiology and Virology in Tbilisi, Georgia, is one of the most well known of the clinics still specialising in this antibacterial therapy. As well as preparations designed for off-the-shelf use for particular disease indications, the institute has a large bacteriophage collection that can be screened against bacterial pathogens from patient samples to create personalised treatments.
For phage therapy to become accepted in modern Western medicine, there are several challenges that must be addressed, the first of which may be to definitively prove safety and efficacy. Perhaps the first safety trials were performed by d'Herelle, who administered phage to himself as well as to family members, noting no adverse effects from the preparations[4].
As a result of the discontinuation of phage therapy in the first half of the 20th century, safety and efficacy testing did not evolve concomitantly with the more rigorous clinical testing standards, which now include blind or double-blind trials with appropriate controls and strict statistical analyses. Accordingly, the efficacy of phage therapy versus standards of care has never been convincingly demonstrated to Western standards, although new efforts are emerging[5,6].
On this front, the large-scale Phagoburn trial has been funded by the European Union and sponsored by Pherecydes Pharma. Phagoburn, which focuses on phage treatment of infected burn wounds, was launched in 2013, with the first patients entering into the phase I/II clinical study in 2015.
In order to test safety, efficacy and pharmacodynamics, cocktails of around a dozen different phages targeting either Escherichia coli or Pseudomonas aeruginosa were designed to treat enrolled patients identified as carrying these specific pathogens. Additionally, AmpliPhi Biosciences, working with the University of Adelaide and Flinders University, recently dosed their first patient with phages targeting Staphylococcus aureus in a phase I safety trial at the Queen Elizabeth Hospital in Adelaide, Australia[7].
The design and implementation of these types of trials will undoubtedly prove critical to moving the technology into modern medicine.
Beyond safety and efficacy trials, potential phage therapies may need to overcome other hurdles, including the release of endotoxin or other toxic bacterial products when infected bacteria rupture. Other issues are the emergence of bacterial resistance to phages, bacterial strain coverage, pharmacokinetics and how to dose a self-replicating agent, as well as the patient immune responses, which may target the phage when administered into the body.
These challenges are already being addressed to some degree, with some work demonstrating phages designed to kill bacteria with limited endotoxin release[8,9] and the selection for phages with improved residence time in the body[10]. Bacterial strain coverage can be improved using phage cocktails, which have multiple phages able to target different receptors on a bacterium, which could also decrease the likelihood of resistance.
Additionally, phages can be naturally evolved to subvert defensive tactics employed by bacteria that have become resistant to infection, meaning that components of a cocktail that are no longer effective could be re-derived instead of shelved alongside defunct antibiotics.
Furthermore, a scaffold approach for rapidly adjusting the range of susceptible bacteria was recently demonstrated by using a well-characterised phage and modifying the leg-like appendages, called tail fibres, that allow the phage to adsorb to components on the bacterial target's surface.
Modern genetic engineering and fields such as synthetic biology have brought about an entirely new branch of phage therapies, using specially engineered phage designed to exhibit improved efficiency or specificity. By modifying the genetic material that they carry, new functions can be added to these highly efficient DNA-delivery machines. For example, a phage was made more efficient at eliminating bacteria in protective biofilms by adding a biofilm-degrading enzyme to the phage genome that was expressed during phage infection.
Like the famed Trojan Horse, bacteriophages have been designed to introduce DNA that expresses toxic, non-specific DNA binding proteins, restriction enzymes and other lethal products from within recipient cells. Bacteriophages to specifically target antibiotic resistance genes or increase bacterial susceptibility to antibiotics may be useful in conjunction with traditional antibiotic therapies.
Bacteriophages can also be programmed to kill only cells containing a predefined genetic signature.
The field of phage therapy is poised very differently now than it was a century ago. The understanding of phage biology that we have today promises to help us to select bacteriophage cocktail components appropriately, produce and purify them according to suitable standards, and design and execute rigorous clinical trials.
New applications of phages are also emerging. These multifunctional tools may be useful in next-generation diagnostics or to target a person's resident bacteria. Otherwise healthy patients who carry drug-resistant microbes or opportunistic pathogens may benefit from targeted phage therapy designed to prophylactically remove these strains, preventing future infection or spread.
Furthermore, the populations of commensal and non-pathogenic bacteria that make up natural microbial communities, such as the gut microbiome, are being extensively studied and are now known to have profound impacts on human health. Phage may allow us to effect precise changes in these communities to treat a range of human diseases outside the scope of bacterial infections.
Although many challenges remain, the dwindling arsenal of effective antibiotics has begun to stimulate rigorous investigation, research and development into alternative antimicrobials, including phages. Perhaps with continued collaboration between academia, medicine, industry and government, we will be able to evolve this forgotten treatment for use in modern medicine.
Ultimately, this push may help us to incorporate the growing knowledge surrounding the importance of our natural bacterial communities to inform the design of smarter, precision antimicrobials.
References
1) Twort, F. W. An investigation on the nature of ultra-microscopic viruses. Lancet 186, 1241–1243 (1915).
2) d'Hérelle, F. Sur un microbe invisible antagoniste des bacilles dysentérique. Comptes rendus l'Académie des Sci. 165, 373–375 (1917).
3) Summers, W. C. Bacteriophage therapy. Annu. Rev. Microbiol. 55, 437–451 (2001).
4) Summers, W. C. The strange history of phage therapy. Bacteriophage 2, 130–133 (2012).
5) Kingwell, K. Bacteriophage therapies re-enter clinical trials. Nat. Rev. Drug Discov. 14, 515–516 (2015).
6) Sansom, C. Phage therapy for severe infections tested in the first multicentre trial. Lancet. Infect. Dis. 15, 1384–1385 (2015).
7) AmpliPhi Biosciences announces dosing of first patient in phase 1 clinical trial of AB-SA01, AmpliPhi press release, 20 January 2016. bit.ly/1YiwUrU
8) Hagens, S. & Bläsi, U. Genetically modified filamentous phage as bactericidal agents: a pilot study. Lett. Appl. Microbiol. 37, 318–323 (2003).
9) Hagens, S et al. Therapy of experimental pseudomonas infections with a nonreplicating genetically modified phage. Antimicrob. Agents Chemother. 48, 3817–3822 (2004).
10) Merril, C. R. et al. Long-circulating bacteriophage as antibacterial agents. Proc. Natl. Acad. Sci. U. S. A. 93, 3188–3192 (1996).
Timothy Lu is an associate professor leading the Synthetic Biology Group in the Department of Electrical Engineering and Computer Science and the Department of Biological Engineering at MIT.
Robert Citorik is a graduate student in the Microbiology Program at MIT and a member of the Synthetic Biology Group. His research interests include the engineering and application of bacteriophages.