“It's a bit of a dream, but it would be transformative for the way people see vaccines”

Could a new generation of nasal spray or oral vaccines help us block infections at the site of entry to the body? Tom Ireland talks to Professor Ed Lavelle about the challenges of developing mucosal vaccines to prevent COVID-19 and other diseases.
February 8th 2022
Mucosal sites are found at the major interfaces between the inside and outside of the body – for example the surfaces of the lungs, digestive tract, nasal cavity and genital tract in humans.
Bombarded with microbes from the environment every day, these surfaces have a unique immune defence system capable of stopping pathogens reaching cells and preventing infections becoming established. There is even cross-talk between distant mucosal sites in the body, helping one set of exposed tissues prepare for a pathogen encountered by another.
Interest is growing in vaccinations that target mucosal sites because of their potential to block infections at the surfaces where the pathogen tries to enter the body. As the development and roll out of COVID-19 vaccines has shown, even successful intramuscular vaccines do not necessarily prevent mild cases and transmission of disease.
But the unique defence systems which make mucosal surfaces so hostile to pathogens also make them hostile to vaccines too. So far, no DNA, RNA or protein subunit vaccines have been developed that can work at mucosal surfaces yet.
Ed Lavelle is a professor in immunology at Trinity College, Dublin. His research focuses on ways to help new-generation vaccines survive and generate an immune response at the body’s mucosal surfaces. Lavelle is hopeful that key roadblocks to mucosal vaccines will be overcome in the next few years, prompting a surge of interest and investment in this approach from the world’s biggest vaccine developers.
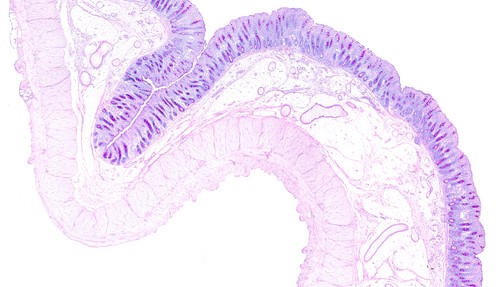 Mucosal surfaces are composed of epithelial cells and mucous which together form a barrier to the external environment. This image of the large intestine shows the mucosal layer in purple with two muscle layers below.
Mucosal surfaces are composed of epithelial cells and mucous which together form a barrier to the external environment. This image of the large intestine shows the mucosal layer in purple with two muscle layers below.Hi Ed. Firstly, how do immunologists define a mucosal site in the body and what is unique about these particular surfaces and tissues?
The principal mucosal sites are the gastrointestinal tract, the respiratory tract and reproductive organs. They are external-facing sites that must deal with everything we eat and everything we breathe in. So they're dealing with a lot of challenges all the time, from the second you're born, and have immune responses that are tailored to those sites. For example, a huge number of the immune cells in your body are in the intestinal tract, and the rules for induction of responses there are quite specific.
The types of antibody responses you get are different at mucosal sites. Some people call the collection of different sites the integrated mucosal immune system, as there are connections between different mucosal sites, but you tend to get the best immune response at the location where you are exposed to the challenge.
What are the challenges of vaccinating via mucosal sites? Why is the development of this idea so far behind intramuscular vaccines?
I think it's probably two reasons. One is that we had intramuscular vaccines with specific adjuvants that worked well, were safe and that had a track record of protection. So there's probably a degree of conservatism – why would you try something different?
Secondly, it's more difficult, as we don't have adjuvants [molecules that help vaccines elicit a strong immune response] that work well at mucosal surfaces. Your spleen and lymph nodes don’t see a lot of microbial components most of the time, whereas the gut sees this stuff every day of your life – it's loaded up with microbes. That's why you can't just translate what's been given by injection to mucosal surfaces. It’s not like your immune cells in the gut have been turned off to respond to these molecules, but they just respond differently.
The ideal vaccine is always going to be an oral vaccine, but you have a really low pH in the stomach, loads of proteases, a thick mucus layer, and a huge dilution factor, and there's no validated adjuvants that work in that environment. Without suitable adjuvants, all the progress that's happened in injectable vaccines – moving from live attenuated and killed vaccines to DNA, RNA and subunit vaccines, hasn't happened at all for oral vaccines or nasal vaccines.
So you have to solve several problems simultaneously. You've got to protect the antigen, get it to the right place intact, and have the right adjuvant all at the right time. You could create a nice capsule that protects the antigen, but then the immune system doesn't care without the correct type of immune activation.
Then another issue is how you assess the response. If you have an injectable vaccine you know that blood-circulating antibodies and circulating T cells are probably a good readout for what's happening. If you're saying the main readout that you want for a mucosal vaccine is local IgA (antibodies found in particularly high amounts at mucosal sites), people need to either volunteer to give you a biopsy or mucosal secretions (e.g. nasal washes, saliva, faecal samples). If it's resident T cell populations then you need to get a biopsy too although new approaches are being investigated such as measuring responses in bronchoalveolar fluid or nasal brushes.
 There are currently eight oral vaccines licensed for use, targeting cholera, salmonella, poliovirus and rotavirus, and one intranasal spray vaccine for influenza. To date, only live attenuated and inactivated vaccines have proved successful platforms for mucosal vaccine design. The major advances seen with injectable vaccines, such as adjuvanted subunit antigens, RNA and DNA vaccines, have not yet been translated into licensed mucosal vaccines.
There are currently eight oral vaccines licensed for use, targeting cholera, salmonella, poliovirus and rotavirus, and one intranasal spray vaccine for influenza. To date, only live attenuated and inactivated vaccines have proved successful platforms for mucosal vaccine design. The major advances seen with injectable vaccines, such as adjuvanted subunit antigens, RNA and DNA vaccines, have not yet been translated into licensed mucosal vaccines.Another one of the advantages with injection is you formulate the vaccine in a very refined way. It has exactly the characteristics you want it to have and then it goes into your muscle in exactly the manner you want. Once you go mucosal, especially orally, you have less control over the vaccine components after delivery.
I think people have for a long time thought all those challenges are a bit too daunting. That's changing though and I think in the next five or ten years, we're going to see a massive leap. We and other groups are starting to see molecules that look promising.
What has changed?
The amount of money that's going into development. With RNA vaccines, there were a number of major challenges there to solve that may have seemed unsurmountable, but they were cracked, and the outcome is amazing. This shows that with the right ideas, and the right amount of funding, we can accelerate processes and do something that was inconceivable.
Now there is a spotlight on transmission-blocking vaccines for COVID, this might be the thing that really unlocks this. People are realising the only way to eliminate the issues we have, or really get on top of them, is to stop people passing the virus on. I'm hoping that if you see one nasal vaccine being approved, or one oral vaccine with a subunit antigen, then that conservatism will dissipate.
How would a mucosal vaccine for COVID-19 complement existing vaccine approaches?
There are two potential approaches. As I mentioned, there is interest in a vaccine that is, in the case of COVID, given nasally from the beginning to induce local responses and try to block infection.
Or there is what we call a “prime and pull” approach, where you get a really strong response by injection, and then you have something that will be able to pull those cells to mucosal surfaces and hopefully retain them. You get the benefits of a potent response from the injection, but the possibility of giving a nasal boost or oral boost to the same populations might then give you greater blocking.
Hopefully, by the end of this year, globally we will be vaccinated to a really high level, so we’re not talking about naive populations. But having a vaccine that's non inflammatory, that avoids needles – where you could say to people if you get this nasal spray from the pharmacy every October, you will not get COVID this winter, even mildly – I think that would appeal to a lot of people. It's a bit of a dream, but it would be transformative in terms of the way people see vaccines.
How else might the field develop in the coming years?
A heat stable oral vaccine would be the ideal way to vaccinate dispersed rural populations in places where there isn't a great infrastructure. You're introducing a set of additional challenges, but if you could go around with a box of tablets in the back of a truck that would transform vaccination.
Now that's extremely difficult but it does offer something that can’t be done by injection. The problem is that heat stability may be easy to talk about, but it's extremely difficult to achieve with existing formulations. In the context of mRNA vaccines, even an oral vaccine that you could leave sitting in the fridge and that people could take and keep in their own fridge might be transformative as well.
Ed Lavelle is professor of immunology at Trinity College Dublin and an internationally recognised leader in the field of vaccine adjuvants.
Lavelle, E.C., Ward, R.W. Mucosal vaccines — fortifying the frontiers. Nat Rev Immunol (2021).